Page contents
Lewy body dementia is the second most common cause of neurodegenerative dementia.
According to Dementia UK, Lewy body dementia accounts for about 10-15% of dementia cases, which means that about 100,000 people in the UK are living with the condition.
Rachel Thompson, Consultant Admiral Nurse for Lewy body dementia at Dementia UK, said in a webinar as part of The Alzheimer’s Show: “Lewy body dementia is often unrecognised and undiagnosed or mixed up with other conditions.
“A lot of people still have great difficulty with getting an accurate diagnosis, perhaps due to the slightly different features that people with Lewy body dementia can experience, such as poor balance, hallucinations and delusions and disturbed sleep. People often retain insight in their condition and memory may be less affected in early stages.”
What causes Lewy body dementia?
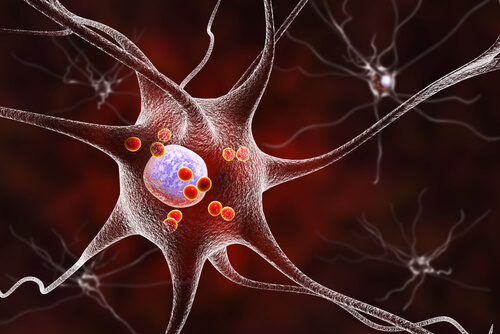
Like other forms of dementia, Lewy body dementia is caused by a build up of proteins in the brain. In this condition, the protein is called alpha-synuclien and clumps together to form Lewy bodies. Lewy bodies were discovered by Friedrich Lewy, a German neurologist in 1912.
Lewy bodies can kill the neurons as well as preventing neurons and neurotransmitters from functioning. This means that the brain cannot send messages between cells effectively and will lose certain functions as cells die.
Types of Lewy body dementia and the connection to Parkinson’s disease
The presence of these alpha-synuclien clumps is called Lewy body disease. Lewy body disease can cause Parkinson’s disease and dementia with Lewy bodies. Around 30% of people with Parkinson’s disease go on to develop Parkinson’s disease dementia. Dementia with Lewy bodies (DLB) and Parkinson’s disease dementia (PDD) are the two types of Lewy body dementia (LBD).
Which type of dementia somebody gets depends on which part of their brain the Lewy bodies are present in.
The mid-brain and brain stem are parts of the brain that control movement, sleep and the nervous system. When Lewy bodies develop here, this can result in Parkinson’s disease.
The cerebral cortex, limbic cortex and hippocampus manage memories, emotions, information processing and language. A build up of Lewy bodies in these areas of the brain can lead to dementia with Lewy bodies.
Somebody can experience both dementia with Lewy bodies and Parkinson’s disease, if they have Lewy bodies in the upper and lower parts of their brain.
Symptoms of Lewy body dementia
The order of which symptoms appear can indicate which form of Lewy body dementia somebody has. Ms Thompson explained in the webinar: “With dementia with Lewy bodies, the cognitive features that appear first or alongside motor symptoms, whereas with Parkinson’s disease dementia, it’s the motor symptoms that come first.”
Symptoms can include:
Cognitive impairment symptoms (these usually fluctuate drastically):
- Poor concentration
- Confusion
- Difficulty processing information that they are receiving through their senses
- Problems with analysing and problem solving
- Some memory issues
Neuropsychiatric symptoms:
- Recurrent complex visual hallucinations
- Delusions
Motor symptoms associated with Parkinson’s disease
- Shaking hand
- Slow, stiff movements
Many people also experience insomnia and REM sleep behaviour disorder years before any other symptoms present. Symptoms of this disorder can include:
- Moving during sleep in response to what is happening in a dream. This could be in bed or sleepwalking
- Talking and laughing during sleep
Many healthcare professionals use the DIAMOND-Lewy management toolkit to assess and diagnose Lewy body dementia, and which type of LBD a person has.
Treatments for Lewy body dementia
As with all forms of dementia, there is no cure, but some treatments can help people to manage or ease their symptoms. These include occupational therapy, physiotherapy, dementia therapies such as music therapy, home adaptations and various medications.
Medication can include antipsychotics, such as haloperidol. Ms Thompson explained: “About 50% of people with Lewy body dementia can have a severe reaction to antipsychotics. These are the medications that are often given when people have things like hallucinations and delusions. Antipsychotics should generally be avoided and other non – medication approaches tried first but if someone is very distressed by hallucinations; specific ‘atypical’ antipsychotics can be tried. These should be introduced gradually at small doses and with very careful management and close monitoring so that we’re sure that the person isn’t going to react badly.”
Find your ideal care home
- Explore a wide range of care options and facilities
- Read independent ratings and reviews
- Connect directly with care homes to book a tour and discuss your needs