General Election: Care campaigners demand improvements for older people
As political parties of all persuasions gather their forces for the final couple of months of campaigning, carehome.co.uk spoke to a number of care providers and charities about what they want the next Government to do to improve the adult care sector.

Not only is this a critical time for health and care services, but the number of older people in the UK is predicted to increase by more than five million over the next two decades. The pressures on the whole system have never been greater – so it is vital that that the new Government gets to grips with the social, financial and health problems.
From the organisations consulted, certain common themes emerged – most notably the problems in the NHS, joining up health and social care, shortages in funding and qualified nurses, and, above all, a predicted woeful lack of care workers.
Power of grey vote
Despite the needs of older people not being adequately met at the moment, they will be able to make a point come election time. Leading not-for-profit provider of housing and care for older people, Anchor, which is actively campaigning for a minister for older people, is warning politicians that they cannot take the grey vote for granted.
Its recent YouGov survey of 2,000 Brits aged 55 and over revealed a shift in political alliance as nearly a quarter (24 per cent) of those planning to vote said they are not going to vote for the same party they voted for in the 2010 election and nearly a fifth (19 per cent) are undecided as to whether the same party will have their allegiance this May. Indeed, grey voters could hold the key to securing vital seats in the upcoming general election as a staggering 93 percent of older people said they will definitely or probably vote on 7 May.
It is to be hoped therefore that political parties will factor in some sensible solutions to help solve the current crisis. As Jane Ashcroft, chief executive of Anchor, says: “The lack of action on health and social care provision is yet another example of where the country's leaders are failing to take action on an issue that concerns older people.
"This political apathy is disastrous both for the older people currently being failed by the system, and for future generations who deserve support in later life.”
Transparency and problem-solving
Simon Bottery, director of policy and external relations for Independent Age, a leading charity offering information and advice to older people, their families and carers, says: “We hope to see the political parties be honest with the electorate about issues affecting health and social care in this country. We would particularly like the election campaign to reveal the true scale of political parties’ ambitions for funding and integrating health and social care.
“It will be particularly interesting to listen to parties outline how they plan to plug the so-called £30bn black hole in the NHS’ finances before the end of the next parliament in 2020.
“We hope that during the election campaign the parties discuss the current decline in the number of older people receiving local council-funded care, whether they plan to change this and also address the amount of funding that councils currently receive.
Government involvement essential
Care England, a registered charity and a leading representative body for independent care services in England, very much puts the onus for improvement on Government. Its 2015 manifesto sets out a number of ways in which it feels that the Government that comes to power following May’s election can act to establish an outcomes-based system of health and social care.
This includes the wish for genuine collaboration between providers and commissioners in which fees are agreed that will enable vulnerable individuals to be supported, with providers being enabled to financially reward staff for delivering high quality care. Also on the Care England agenda is the need for real partnership working between providers across health and social care. It believes GPs should provide enhanced healthcare in care homes, and the NHS should take advantage of the increased capacity across the independent sector in times of service pressure.
In its view, the adult social care sector will need another one million employees within the next decade, and such a huge increase will require investment from Government that supports provider-led innovation that maximises productivity. In addition to this, Government can add care home nurses to the Shortage Occupation List, which would ease the nursing shortages currently being experienced across the sector.
Person-centred care
Some providers believe that person-centred coordinated care is essential for the development of health and social care over the next five years. According to Jules Acton, director of engagement and membership for National Voices, a coalition of health and social care charities in England: “Key to this is making the things that matter to people one of the key organising principles for services. We want to see this changed with people in all settings – including care homes - and families having as much control over decisions as they would like.”
Related to this, National Voices would like to see all people in care homes experience good care and support planning as well as access to services outside the home. These include good access to health professionals, such as GPs and dentists and also to leisure and other activities that bring meaning to their lives and support people’s wellbeing.
National Voices would also encourage professionals to consider if advance care planning is appropriate from the point a person enters a care home. Mr Acton explains: “Currently advance care planning is often triggered by an incident such as a fall yet, in many cases, it will be most appropriate and effective to embark on this process at the point people enter the homes when they are at a point when they can have conversations about their own wishes with staff who have training in holding this kind of discussion.
Like Independent Age, National Voices supports secure funding for both health and social care need. Its members are calling on the next Government to support a well-funded health and care sector with a guaranteed financial settlement of at least five years’ duration. In particular, it wants to see real terms increase for social care funding, sufficient to deliver on the policy goals of the Care Act 2014. This means funded social care should be available for larger numbers of adults with assessed needs. And social care should be available free for people needing end of life care.
The organisation also urges the next Government to resist any further extension of charging for health and care services, since this undermines the principle of services delivered according to need rather than ability to pay, and reinforces health inequalities.
Pragmatic reforms
Some care providers feel that the very basics of the system need to be addressed. Managing director of Penrose Care, an innovative London-based home care provider, Robert Stephenson-Padron, stresses the need for a pragmatic approach. He says: “The next Government needs to continue efforts to reform our ailing social care system. Funding issues are well known, but the actual mechanics of reforms need reforming as the current approach is frankly, wrong-headed.
"New reforms need to both focus on what is effective and remove the incredible amount of discretion in many regulations, which cause a lot of undue paper work and confusion.
“For instance, rather than providing broad categories of goals such as [asking the question] is a provider ‘responsive’, which necessitates compiling loads of paper work to indicate compliance, different quality ranking should be based on the implementation of specific, concrete, and effective steps checked with questions. In other words, the goals should be more tightly defined. “Rather than asking a broad question such as, is a provider safe?, ask for instance, ‘do they fulfil Schedule 3 pre-employment checks and does the provider have an occupational sick pay scheme to incentivise workers from not going to work with vulnerable people when they are ill?’ ” says Mr Stephenson-Padrow. He believes that the more concrete effective steps a provider implements - which can be checked via email or telephone rather than expensive physical visits - the better their quality ranking. “Removing excessive discretion from regulations and focusing on concrete steps we generally agree lead to better care will reduce the paper work burden of providers and also remove administrative burdens of the regulator, allowing both to focus on tasks that genuinely improve quality, and also genuinely improve quality in itself. Paper work will not solve our numerous care crises, indeed it gives us less time to respond to them,” he says.
“Implementing such a light but effective regulatory system would provide the regulator with the bandwidth to implement a more engagement-led approach to the sector rather than a compliance-led approach. The goal should be for all providers to be ‘Outstanding’ and the regulator should therefore act as a consultative partner rather than a ‘catch you out’ agent.
“I would direct Parliament to look at how Citizens UK has extremely effectively promoted business ethics across the UK as a model of how our regulation in health and social care should be pursued.”
Latest Features News
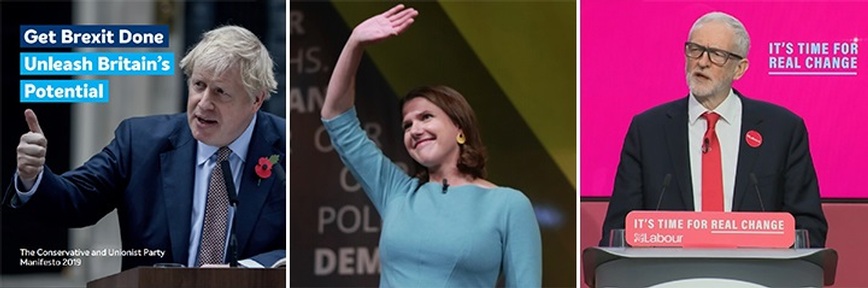 25-Nov-19
2019 Election: Boris Johnson leaves social care in 'too difficult box' but Labour vows to end 'crisis'
25-Nov-19
2019 Election: Boris Johnson leaves social care in 'too difficult box' but Labour vows to end 'crisis'
 18-Oct-19
Podcast: Wendy Mitchell and dementia: 'My biggest fear is not knowing who my daughters are'
18-Oct-19
Podcast: Wendy Mitchell and dementia: 'My biggest fear is not knowing who my daughters are'
 27-Sep-19
Exclusive: Care minister backs care workers' call for time off to grieve and attend funerals
27-Sep-19
Exclusive: Care minister backs care workers' call for time off to grieve and attend funerals
 19-Sep-19
Podcast: Gyles Brandreth says poetry helps ward off dementia
19-Sep-19
Podcast: Gyles Brandreth says poetry helps ward off dementia
 30-Aug-19
Edinburgh Fringe funnyman joins comics facing toughest audience at care home gig
30-Aug-19
Edinburgh Fringe funnyman joins comics facing toughest audience at care home gig