Dementia simulation helps to improve care worker practice
The growing number of people living with dementia has led to an increase in the demand for care that is both knowledgeable and appropriate.
Dementia care is often considered a key requirement in care homes across the UK and can prove crucial to people living with the condition.
Patients, care home residents and their loved ones need to be able to make informed decisions about their care and know that care is being delivered by skilled and qualified care professionals.
Oxford Brookes University is one of the latest organisations that has devised a training programme to help to support people with dementia by ensuring that they are supported by empathetic staff and care workers as they go about their daily lives, both in and outside of care homes.
The university's Dementia Simulation Training provides commissioners, healthcare professionals and care staff with an increased awareness of what people living with dementia experience on a day-day-day basis.
Teaching people how to provide emotional support to those with dementia
Rozz McDonald is an occupational therapist and the Dementia Simulation Training facilitator. She commented: “Oxford Brookes uses simulation as a teaching tool, it’s widely used with medics and doctors who use manikins to practice skills such as taking blood and basic life support.

"We've developed the idea of simulation further by using an actor to allow people to practice real skills with a real person who can respond to them. Often patient safety and communication can be difficult to teach when using simulation in a classroom as other students take on the role which can be difficult if that person hasn’t got the physical problems that you’re trying to simulate. By using actors to simulate patients, we can teach people how to support their patient or resident with the emotional aspects associated with dementia and ageing, such as behaviour, communication and distress.
"The Dementia Simulation suit helps to simulate ageing and impairs the movement of those wearing it, simulating some of the typical difficulties that people experience in older age, showing you how tiring it is not to be able to move fully, stopping you being able to freely move your joints, making it difficult to feel and move your hands and fingers and grip things. It also has a back piece that gives you a curvature of the spine so you can’t stand up and googles that give you a yellowing vision to replicate loss of sight and peripheral vision, typically associated with cataracts, while ear plugs can impair your hearing and awareness of your surroundings.”
A range of schemes are already in operation to increase understanding and raise awareness of what it is like to live with dementia including, Training2Care’s Virtual Dementia Tour which puts participants in an environment that someone with dementia may experience on a daily basis. While Alzheimer's Society's Dementia Friend programme encourages people to become ‘dementia-friendly’ and to create dementia inclusive communities.
The training package has been carefully designed for health and care staff and volunteers to build dementia awareness and to gather insights into the requirements of people living with dementia, which may not otherwise be considered. Furthermore the training helps participants to develop new skills to support people with dementia more effectively.
Helping organisations to develop new skills and provide effective support
Ms McDonald continued: "Dementia Simulation Training is delivered over one day and allows participants to develop an awareness of what life is like with dementia based on experiential learning, and provides them with the opportunity to reflect on their experiences and the needs of their own local communities and the areas they work in."
The training can help organisations to progress towards the Government’s National Dementia Strategy, which sets out 17 key recommendations to help health and care services to deliver compassionate care to all patients and residents. The strategy focuses on three themes: to raise awareness and understanding, to aid early diagnosis and provide support and to help people to live well with dementia.

Ms McDonald said: “During the training, participants are given a series of tasks, such as getting in and out of the chair, walking up and down the stairs and going out into corridors and finding signs and navigating their way to the toilets as if they were a person with dementia visiting a hospital or care setting. People really begin to appreciate how difficult it can be and how it can affect you as a person and your behaviour. We ask people to do a care giving task on each other and they appreciate how life is for someone who is older with impaired mobility and it can help people to become more empathic and change the way they approach different settings and scenarios.
“We’ve held the training in care homes, acute hospital settings and with community staff. Most people are affected quite deeply and realise that they need to give people more time.”
The training is part of the Continue Professional Development (CPD) profile within the Department of Applied Health and Professional Development and the Department of Nursing, offering study and support opportunities to professionals in areas including: cancer care, palliative care, surgical nursing and dementia.
People who participate in the course can use the ageing suit and learn about assistive technology, dementia friendly environments, telecare, environmental adaptations and equipment and activities to help people with dementia to feel settled and engage and to help them find things to do if they’re very mobile. Training also offers information on the clinical aspects of dementia care.
'Good nursing practice is about putting yourself in that person’s position'
Tricia O’Leary is the manager of specialist dementia care home, Vale House in Littlemore, Oxford. Recently some of the staff at the not-for-profit home participated in the Dementia Simulation Training. She commented: “I did my training in the 70’s and have been nursing for about 40 years and it was the best learning experience that I’ve ever had in terms of putting myself in the place of someone who is old, who may have memory problems and whose eyesight might be failing.

“Good nursing and good nursing practice is about trying to put yourself in that person’s position and I found it really beneficial– so good that we’re going to buy our own suit for use here so that all of our staff can have that experience so that we can really empathise with our residents.
“The training is unique in that it really puts you in the shoes of the person who you are looking after and it has given us a fresh insight into what it really is like to be old, a bit arthritic and have poor eyesight and hearing. All of our residents at Vale House have dementia, so on top of some the natural changes that occur with ageing, being confused and maybe not understand your surroundings has allowed us to help our residents to get through their days and nights.”
Ms McDonald added: “The Dementia Simulation Training programme was designed to provide people with some skill based opportunities to allow them to practice their skills. We are hoping to embed this training in the students' training so they get that before they qualify.
“We know that if you can affect people, then you can influence people’s practice, which is why we conduct experiential training.”
For more information on the training, visit: http://www.chc.brookes.ac.uk/training/dementia-simulation or email: dementiaworkshop@brookes.ac.uk
Latest Innovative Care News
 13-May-19
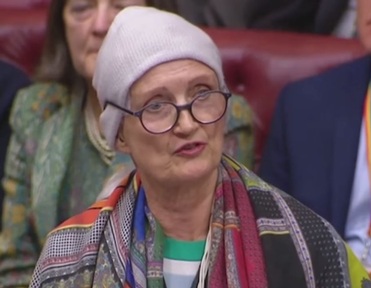
'Pink drink' brain cancer treatment rolled out across NHS in memory of Baroness Jowell
13-May-19
'Pink drink' brain cancer treatment rolled out across NHS in memory of Baroness Jowell
 25-Apr-19
Louis Tomlinson helps 83-year-old who lost wife to dementia complete bucket list
25-Apr-19
Louis Tomlinson helps 83-year-old who lost wife to dementia complete bucket list
 22-Mar-19
UK's top care home handyman takes residents to pub for pie and pint
22-Mar-19
UK's top care home handyman takes residents to pub for pie and pint
 12-Feb-19
Michael McIntyre's jokes tested to see if they stop elderly catching flu
12-Feb-19
Michael McIntyre's jokes tested to see if they stop elderly catching flu
 07-Jan-19
'We were lucky to find it': Family's delight as care home is rated Outstanding
07-Jan-19
'We were lucky to find it': Family's delight as care home is rated Outstanding