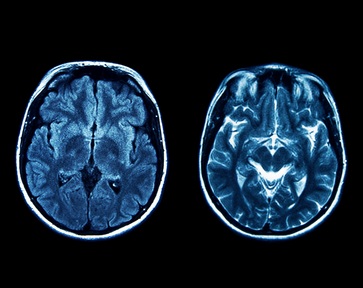
Protein discovery could 'reverse' symptoms of Alzheimer's disease
Alzheimer’s symptoms could be reversed by restoring a protein which is missing in the brains of those living with dementia, according to new research published in the journal Proceedings of the National Academy of Sciences (PNAS).
Researchers at the University of Glasgow and the Hong Kong University of Science revealed that increasing levels of the protein IL-33 reversed symptoms within a week during a trial on genetically-engineered mice.
Dr Simon Ridley, director of research at Alzheimer’s Research UK, said: “The role of the immune system in Alzheimer’s disease and other causes of dementia is a promising area of focus for drug discovery efforts.
“This early research in mice highlights a way of boosting the immune system to clear a toxic Alzheimer’s protein, but we’ll need to see the results of clinical trials before we’ll know whether this approach could one day help people living with the disease.
“Alzheimer’s Research UK is investing in drug discovery projects in the UK and internationally, taking the most promising ideas from the laboratory and accelerating their progress towards the clinic. As there are no treatments that can halt the damage caused by Alzheimer’s disease, it’s important that many different approaches are tested in the hunt for new, effective medicines.”
There are currently 850,000 people living with dementia in the UK which is expected to rise to one million by 2025 and two million by 2050. However, there are currently no treatments to prevent or reverse dementia.
The trial tested the effects of a protein called IL-33 on a strain of mice genetically-engineered to mimic the development of Alzheimer's disease in humans.
The IL-33 protein occurs naturally in the human brain and spinal cord, yet previous studies have shown that it exists in much lower concentrations in the brains of people living with Alzheimer's disease compared to healthy individuals.
They found that mice injected with IL-33 had improved nerve cell communication and performed better on a particular type of memory test.
They also found that IL-33 could decrease the amount of amyloid – a toxic protein found in Alzheimer’s – in the mouse brain, as it triggered immune cells to remove amyloid clumps.
Professor Eddy Liew, fellow of the Royal Society, who co-directed the research, said: “Alzheimer’s disease currently has an urgent unmet clinical need. We hope that our findings can eventually be translated into humans.
“IL-33 is a protein produced by various cell types in the body and is particularly abundant in the central nervous system (brain and spinal cord). We carried out experiments in a strain of mouse (APP/PS1) which develop progressive AD-like disease with ageing.
“We found that injection of IL-33 into aged APP/PS1 mice rapidly improved their memory and cognitive function to that of the age-matched normal mice within a week.”
The study could lead to human clinical trials on Alzheimer's patients as early as next year, although the scientists behind the project warn that there is ‘a long distance’ to go to turn the success in the mouse study into an effective treatment in humans.
Professor Liew added: “The relevance of this finding to human Alzheimer’s is at present unclear. But there are encouraging hints. For example, previous genetic studies have shown an association between IL-33 mutations and Alzheimer’s disease in European and Chinese populations. Furthermore, the brain of patients with Alzheimer’s disease contains less IL-33 than the brain from non-Alzheimer’s patients.
“Exciting as it is, there is some distance between laboratory findings and clinical applications. There have been enough false ‘breakthroughs’ in the medical field to caution us not to hold our breath until rigorous clinical trials have been done. We are just about entering Phase I clinical trial to test the toxicity of IL-33 at the doses used. Nevertheless, this is a good start.”
Latest News
 29-Jul-24
Dementia Bus gives carehome.co.uk staff insight into life with dementia
29-Jul-24
Dementia Bus gives carehome.co.uk staff insight into life with dementia
 01-Mar-24
Find out the top care homes in 2024
01-Mar-24
Find out the top care homes in 2024
 21-Mar-23
UK's top care homes in 2023 revealed
21-Mar-23
UK's top care homes in 2023 revealed
 03-Jan-23
carehome.co.uk launches free care helpline
03-Jan-23
carehome.co.uk launches free care helpline
 13-Dec-22
5 mins with Emily Whitehurst, chief operating officer for Constantia Healthcare
13-Dec-22
5 mins with Emily Whitehurst, chief operating officer for Constantia Healthcare