Social interaction in care homes reduces aggression in people with dementia
Just one hour of social interaction combined with personalized care, can reduce anxiety and aggression in care home residents with dementia, according to a new study.

A large-scale trial led by the University of Exeter, King’s College London and Oxford Health NHS Foundation Trust found that this approach also saves money.
The new study, funded by the National Institute of Health Research upskilled key care home staff to deliver person-centred care. This included talking to residents about their interests and involving them in decisions around their own care.
Professor Clive Ballard, of the University of Exeter Medical School, who led the research which has been published in the journal PLOS Medicine, said: “While many care homes are excellent, standards still vary hugely. We have previously found that the average amount of social interaction for people with dementia was just two minutes a day. It’s hardly surprising when that has a knock-on effect on quality of life and agitation.
“Our approach improves care and saves money. We must roll out approaches that work to do justice to some of the most vulnerable people in society. Incredibly, of 170 carer training manuals available on the market, only four are based on evidence that they really work. That is simply not good enough – it has to change.”
The trial involved more than 800 people with dementia across 69 care homes in South London, North London and Buckinghamshire. Two ‘care staff champions’ at each home were trained over four day-long sessions.
Dr Jane Fossey from the Oxford Health NHS Foundation Trust, said: “Taking a person-centred approach is about getting to know each resident as an individual - their interests and preferences - and reflecting these in all aspects of care. It can improve the lives of the person themselves and it can be rewarding for carers too. We’ve shown that this approach significantly reduces agitation and saves money. Rolling out the training nationwide could benefit many other people.”
The results are the findings of the Improving Wellbeing and Health for People with Dementia (WHELD) trial, the largest non-pharmacological randomised control trial in people with dementia living in care homes to date.
Dr Doug Brown, director of Research at Alzheimer’s Society, commented on the study, saying: “Seventy per cent of people living in care homes have dementia, so it is vital that staff have the right training to provide good quality dementia care.
“A person-centred approach takes into account each individual's unique qualities, abilities, interests, preferences and needs. This study shows that training to provide this type of individualised care, activities and social interactions can have a significant impact of the well-being of people living with dementia in care homes. It also shows that this kind of effective care can reduce costs, which the stretched social care system desperately needs.
“Alzheimer’s Society is committed to improving dementia care through research. That means getting interventions like this put into practice, and funding further research to improve the quality of life for people with dementia in their own homes, care homes and hospitals.”
Latest Innovative Care News
 13-May-19
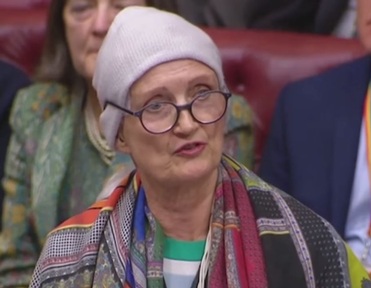
'Pink drink' brain cancer treatment rolled out across NHS in memory of Baroness Jowell
13-May-19
'Pink drink' brain cancer treatment rolled out across NHS in memory of Baroness Jowell
 25-Apr-19
Louis Tomlinson helps 83-year-old who lost wife to dementia complete bucket list
25-Apr-19
Louis Tomlinson helps 83-year-old who lost wife to dementia complete bucket list
 22-Mar-19
UK's top care home handyman takes residents to pub for pie and pint
22-Mar-19
UK's top care home handyman takes residents to pub for pie and pint
 12-Feb-19
Michael McIntyre's jokes tested to see if they stop elderly catching flu
12-Feb-19
Michael McIntyre's jokes tested to see if they stop elderly catching flu
 07-Jan-19
'We were lucky to find it': Family's delight as care home is rated Outstanding
07-Jan-19
'We were lucky to find it': Family's delight as care home is rated Outstanding